Introduction
Since the 90s, the management of chronic pain has become a public health priority. Held by three national plans for pain (in 1998-2002, 2002-2005 and 2006-2010), pain education became a specific education for students in medicine and nursing schools. Gradually, specific training in chronic pain is recommended and required for nurses working in pain consultations. In addition, their missions become more complex with nursing care activities, organization of cares, research and teaching.
The nurse working in tertiary structure of chronic pain (Structure Douleur Chronique: SDC) received an initial training and a specialized training in pain, usually a university degree. Her missions include: 1) the realization of a multidimensional pain assessment, 2) participation in multiprofessional care of the patient, and 3) the establishment of technical care and support. This allows us to offer personalized care to the patient with chronic pain. Skills of nurses in SDC enriched over the years with new degree programs. This is hypnosis, psychocorporal practice or therapeutic education (1). These techniques are essential to support the patient as a whole person, diversifying the supply of care: this is what makes the specificity of SDC (2). The initial evolution is moving towards an integrated academic training in the “bachelor- master- doctorate” process.
Undergraduate education
The program
Initial training on chronic pain begins during courses at the Institute of Nursing Training (Institut de Formation en Soins Infirmiers: IFSI). They are part of the Education Unit called “traumatic process.” It comes from a national program developed in 1992 and is undergoing updated. In this program, pain pathways and typology are described. After an enumeration of various pain scales (one-dimensional and multidimensional scales), levels of WHO regarding analgesics is taught. This initial training in acute and chronic pain is brief: there is no emphasis on the special care both in terms of drug and non -drug treatments or the broader supported person-centred. Each school offers their own training in nursing education according to the national program and it is not uncommon that the share devoted to pain varies from a school to another.
Perspectives and recommendations
Early learning on the awareness of chronic pain is necessary to identify patients at risk of chronicity. It is proposed in the Canadian model (3). Chronic pain is approached through three nursing diagnoses: assessing the physical, emotional and psychological dimensions of the patient. Migraine, neuropathic or abdominal pains are developed as well as treatments such as transcutaneous electrical nerve stimulation or relaxation.
Conclusion
In conclusion, this is no longer a nursing job but nursing professions. This wealth comes from the diversity of services where professional practice and is justified with the creation of the National Order of Nurses. This is especially true in chronic pain because the nurse must have clinical skills, technical know-how and organizational capacities.
Postgraduate development in nursing
Pain nurse specialists
The current training is no longer sufficient to meet the multitude of practices, knowledge, protocols, experiences, leading nurses to specialize in continuing education. There are validated educations: interuniversity diploma on acute pain, chronic and pediatric palliative care, university diploma on oncological pain. There are also specific education on hypnosis, music therapy, cognitive behavioral therapy, and psychocorporal practice. Others are not validated to date, such as “touch massage” and all the techniques that have not been scientific proof of their effectiveness.
The French Society for the Study and Treatment of Pain (Société Française d’Etude et de Traitement de la Douleur: SFETD) has set up a nurse commission to promote professional nurse nursing expertise in the field of pain. One of its activities is to organize, nurses universities where are discussed innovative topics such as “nurse consultation and technical communication”, “chronic post-surgical pain” or “evaluation of professional practices”.
Throughout their professional practice, nurses are required to train to use specific equipment “training pump control analgesia”, setting of spinal cord stimulators and intrathecal pumps, use of nitrous oxide. Outside the initial and continuing training, there is actually a continuous learning: teaching patients! Throughout the exercise, nurses also learn by experience. The experience of their elders, their colleagues but also the situations already experienced leading insurance and reinsurance. Exchanges and meetings allow to evolve, to adapt and to respond more appropriately to requests. Patient’s experience, although each story is different, provides specific lighting in a given situation. Each lived experience is unique to the person who lives but it is also common to a certain group of patients with the same pathology. Thus, exposing a situation experienced by a real person or inspired by many patients can illuminate a problem, consider the various possible solutions. Skills-knowledge is acquired without necessarily learned from books. It is this material that naturally leads to therapeutic education consultation for chronic pain.
Roles of pain nurses
Clinical care
The missions of a nurse working in pain clinic is clearly defined by the French Health Authority (HAS) (1). There are:
– Initial patient assessment
– Nursing consultation
– Participation in consultation with the doctor with the completion of patient questionnaire specific questionnaire
– Assessment and monitoring inpatient
– Development of a pain education program for patients, agreed by local health agency
Technical skills are essential such as performing technical procedures:
– Use of nitrous oxide
– Treatment infusions
– Transcutaneous electrical nerve stimulation (TENS),
– Participation in the implementation and monitoring of morphine pumps,
– Participation in implementation and monitoring tests and treatment protocols.
– Psychocorporal practice and patient education are strongly recommended.
Organizational care
According the article L.1112 -4 of the French Public Health Code, each health establishment is required to organize the management of pain for all their patients. (4) Functioning of the Committees for the Fight against Pain (Comité de lute contre la Douleur: CLUD) is a legal requirement. Different members of CLUD represent professions practicing within the institution. The nurse finds its natural place. As pain referent, spots within the hospital are varied. The first is to make the link between CLUD and service connection, to inform caregivers about the recommendations of the institution, medical authorities and the latest legislation regarding the management of pain. Meetings are held regularly referring pain. Information activities are planned within the services. Transversal interventions are possible to explain a specific or new technology for health care teams, handling specific hardware or supporting patients during painful treatments. Next institutions, there is also a mobile pain team whose role is to meet patients and caregivers.
With the reorganization of the different services and the role assigned to each part of health is rarely dedicated specifically and solely to the pain center but rather is in charge of several care units. That is why the pain nurse must be autonomous, both in material management and for organizing his schedule.
Teaching
The nurses working in chronic pain consultation is primarily a main teacher with training in care: analgesia techniques such as morphine pumps, handling or use of nitrous oxide, use of assessment tools, prevention pain related to health care, timely information in the wards including through mobile teams pain, pain training for his institution. It is also a trainer in the training institutes or schools and nursing caregiver, supervision of students (nursing students, students registered in university diploma on pain, midwife student, and pain specialty for physicians) and guidance works graduation. It also participates in university education: the university diploma on pain management, pain specialization (Capacité Douleur or Diplôme d’Etudes Spécialisées Complémentaires in pain and palliative care). Finally, the nurse participates in the conference as “nursing” session at the annual meeting of the SFETD. However, there is no specific training given to direct teaching, which is surprising given the importance of the requested courses.
For the record, the list of University Diplomas or Interuniversity Diploma on pain is available on the website of the SFETD at: www.sfetd-douleur.org and the National Resource Center against the Pain (Centre National des Ressources contre la Douleur: CNRD) at this address: www.cnrd.fr
Research
The nurse working in chronic pain consultation can participate in the research. In general, she is responsible for the overall organization, making appointments, the pain ratings or the installation of a treatment. It is in this case, she participates in clinical trials as a nurse in clinical research. It may also be the investigator of a project. This is possible with a specific financing: Hospital Research Program Nurse and Paramedic (Programme Hospitalier de Recherche Infirmier et Paramédical: PHRIP). However, in the absence of training in research methodology, it is difficult to participate in these projects. This is also the subject of a nurse university of the SFETD. English can also be a barrier, although it is now included in the initial training of nurses. There is a lack of training on the methodology of study and writing an article or estimation for a research budget. Moreover, it becomes even more difficult in non-university hospital or for a nurse in part time. It would be important to develop a pain journal indexed in French. It is important to be indexed on the basis of SEO such as Pubmed or CINAHL, which are a source of funding.
The impact of their role
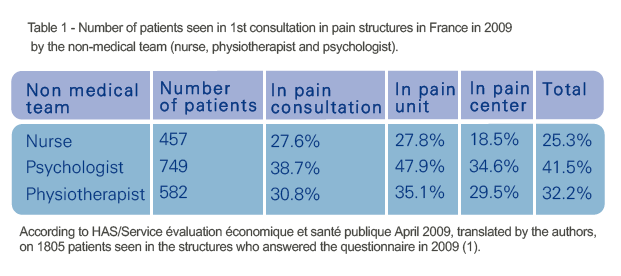
In 2009, the HAS and the SFETD proposed an evaluation of the pain clinics. At this moment, three structures existed: the pain consultation (multiprofessional team), the pain unit (multiprofessional and multidisciplinary team) and the pain centre (with a day hospitalization, neurosurgery, and available invasive technique). On 1805 patients seen in pain structures in France in 2009, 25.3% had a consultation with the nurse (table 1).
In 2005, the SFETD realized a study concerning the pain structures in France. The table 2 presents the proportion of nurse, psychologists and physiotherapist in these structures according the time of work (percentage of a full time work).
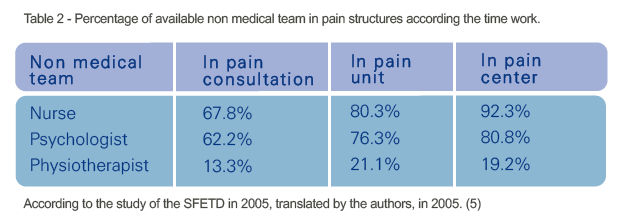
These two works concluded on the importance of the nurse specialized in pain and the importance of her participation in patients’ management. That is why; the multiprofessional evaluation of the pain is an important point for the valorization of a SDC (2).
National developments that help nurse specialists
The evolution of profession tends towards the development of skills to a level of advanced practices. To do this, the law prepare with the appearance of intermediate trades. For this, the creation of a master 2 for nurses is engaged and especially in the future a program on chronic pain management will be available. It would provide access to nurses prescribing certain medications (6, 7).
Moreover, the possibility to imagine that clinical practice guideline can be developed by nurses. This is the case in Belgium where recommendations for nurse was proposed on the management of pain (8).
Conclusion
Pain education for nurse in France was developed in the past two-decades with a richness of activities in clinical care, research, training or organization. The possibility to have a master degree is very interesting economically and the role of the nurse will become more and more important with the advanced nurse consultations (7). However, for the moment, these activities are not well traceability and the financial development is insufficient (9). We hope that the third program on pain will emphasize on the specific mean for SDC.
References
1. HAS, Etat des lieux. Douleur chronique : les aspects organisationnels. Point de vue des structures spécialisées. Argumentaire, 2009.
2. HAS, Evaluation et amélioration des Pratiques Professionnelles. Evaluation du syndrome douloureux chronique en structure spécialisée. Novembre 2009.
3. Phaneuf M, Grondin L. Diagnostic infirmier et rôle autonome de l’infirmière, Sciences Infirmières. Paris: Maloine 2002.
4. Article L1112-4. Modifié par l’Ordonnance n°2010-177 du 23 février 2010 – art. 1
5. Étude pour la Société française d’étude et de traitement de la douleur, Cemka-Eval, Duburcq A, Courouve L. Enquête sur l’activité des structures de prise en charge de la douleur chronique rebelle en 2005. Paris: CEMKA-EVAL 2008.
6. Henart L, Berland Y, Cadet D et al. (2011) Rapport relatif aux métiers en santé de niveau intermédiaire – Professionnels d’aujourd’hui et nouveaux métiers: des pistes pour avancer. Paris: 2011 – www.sante.gouv.fr
7. Gautier JM. Infirmiers ressources douleur et pratiques avancées: mythe ou réalité? Douleur Analg 2012; 25 (3): 136-143.
8. Service publique fédéral, Santé publique, sécurité de la chaine alimentaire et environnement. Recommandations de bonnes pratiques en art infirmier: «rôle infirmier dans la prise en charge, à domicile, de patients adultes souffrant de douleur chronique», 2009.
9. Agnes N, Piano V. Valorisation des activités infirmières en structures douleur chronique. Présentation au 13ème congrès de la SFETD, Paris, 2013.
